Ries Robinson, MD, is the CEO of Rodin Scientific, specializing in the early detection of heart conditions. He also serves as the Chief Innovation Advisor at Presbyterian Healthcare Services, New Mexico’s largest healthcare provider, where he leads initiatives to identify, pilot, and scale innovations that benefit both patients and healthcare providers. His work focuses on reducing the burden on clinicians while empowering patients to take control of managing their health. Dr. Robinson is also a new member of the DocGo Medical Advisory Board.
Healthcare in the U.S. today fails to meet the needs of its key stakeholders. Patients are dissatisfied, physicians are burned out, and payors spend enormous sums on a system that often delivers poor results. It’s clear that healthcare delivery needs to improve—particularly in terms of quality, convenience, and cost.
Chronic care alone accounts for three out of every four healthcare dollars spent. The progression of chronic diseases is not a sudden event. Patients don’t go from being perfectly healthy to requiring hospitalization overnight. Whether it’s asthma, heart disease, or kidney disease, there’s always a progression—a gradual shift from baseline health to a state requiring emergency intervention. If we are serious about improving outcomes, it’s clear that we need to embrace proactive care, intervening at the earliest sign of trouble rather than waiting until a patient ends up in the emergency room.
Think of it like an automatic braking system in a car. The system doesn’t wait until you’re about to crash to activate; it senses when something is off early and applies the brakes before the situation escalates. In healthcare, the same principle should apply: we need to identify and act on subtle warning signs before patients deteriorate.
The Missing Link
Early in my career, I worked at a hospital where we frequently treated patients with heart failure exacerbations—patients we referred to as “frequent flyers” because they were constantly being readmitted. Later, while serving on the board of Presbyterian Healthcare, I witnessed hospitals across the country being penalized for excessive readmissions, a clear indicator that our reactive, crisis-driven model of care was failing. The missing link? Actionable data.
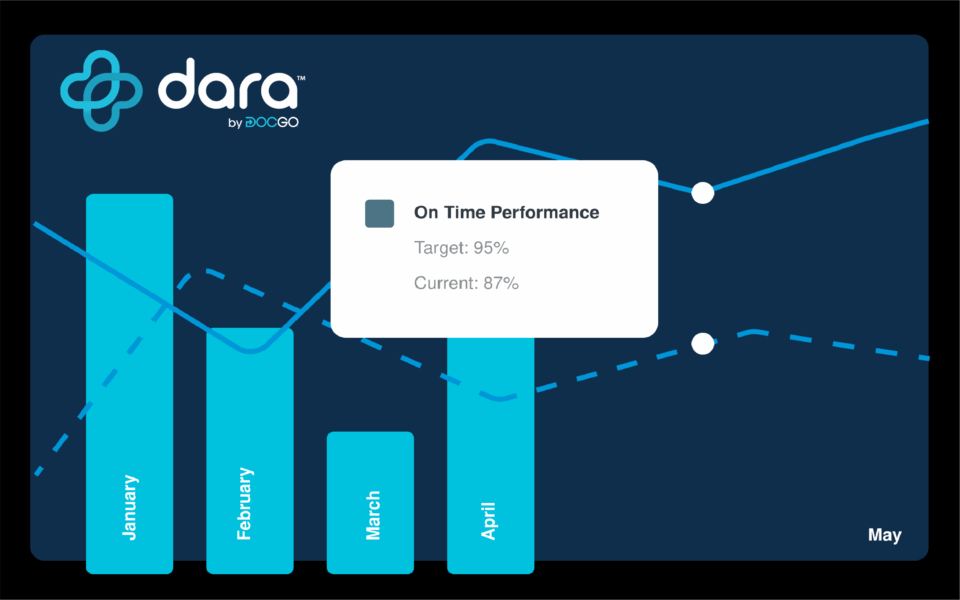
To deliver proactive care across a range of chronic conditions, we need to embrace technology like remote patient monitoring that can detect the subtle warning signs of disease progression, provide actionable data and enable timely intervention.
The Medici Effect
One of my guiding principles is the Medici Effect—the idea that innovation occurs at the intersection of diverse ideas and industries. Too often, healthcare is overly introspective, failing to look beyond its own boundaries for solutions. Right now, one of the clearest lessons from other industries is the need to speed up the transition from innovation to adoption. In healthcare, it’s estimated that it takes an average of 15 years for a new solution to be widely implemented. To put that into perspective, the first iPhone was released in 2007—just over 17 years ago—and we’re already on the 16th iteration! No other industry would tolerate healthcare’s sluggish pace of progress. Yet in our industry, this lag is the norm. If we want to make meaningful change, we must accelerate this process.
Obstacles to Adoption
So, what’s holding back the adoption of technology that provides reliable information about a patient’s health and enables proactive care? One of the biggest obstacles is the misalignment of incentives. The fee-for-service model, which dominates U.S. healthcare, rewards providers for treating illnesses, not for keeping patients healthy. A heart patient generates revenue every time they’re admitted to the hospital, but not when they’re kept out of it. This system doesn’t encourage proactive care; it incentivizes reactive treatment. This misalignment makes it incredibly difficult to shorten the innovation-adoption lifecycle.
No Longer Just An Idea
The future of healthcare lies in proactive, data-driven care—where patients don’t wait until they’re in crisis to receive treatment. But to build this future, we need to realign incentives, remove barriers to adoption, and accelerate the integration of innovative solutions. Without sensors to detect problems early, the “automatic braking system” of healthcare simply can’t function. We can’t afford to wait 15 years for life-saving technologies like advanced remote patient monitoring tools to become standard practice.
By embracing the intersection of diverse ideas, industries, and technologies, we can drive innovation from theory into practice. Healthcare doesn’t need more ideas. It needs solutions that deliver tangible outcomes—and it needs them now. The stakes couldn’t be higher, and the time to act is now. Because innovation without action isn’t progress—it’s just potential left unrealized.